• Breast Access • Best Latch Possible • Be Kind •
Dr. Laura Kent-Davidson, ND, IBCLC
While living in Bangkok last year, I had the great pleasure of sharing with a large group of parents-to-be at Bumrungrad International Hospital. The topic of conversation was getting off to the best start possible with breastfeeding– a topic close to my heart and one that many expecting families ask me about in my private practice. Empowering families with knowledge and tools for those early days postpartum goes a long way in supporting the learned process of breastfeeding for everyone involved. While there are many things to consider, I think it can all be boiled down to 3 key areas, what I call the 3 B’s for breastfeeding.
The 3 B’s for Breastfeeding
1. | Breast Access
Sounds obvious but there are a lot of potential barriers that can be put up in those early days (often unintentionally!), while we are establishing the breastfeeding relationship. Things like not rooming in/having baby sleep far from you, swaddling and waiting until the baby is crying before offering the breast, can all be potential barriers to breast access in those early days. Not only are we talking about physical proximity here, but it is also about following the infant’s unique cues and appreciating their unique needs. Not all babies are the same as far as their feeding ability and feeding frequency so breast access gives them and their caregivers a chance to figure it all out. We want to allow them to wake when they need to, whether that is an hour after their last feed or a few hours (swaddling can potentially interfere with as it promotes longer periods of sleep), and we want to respond to their early signs of hunger as we help them establish a sense of trust to our responsiveness. What we should then focus on is lots of skin-to-skin time to allow the infant to wake up on the mother’s chest and move their way down to the breast while calm.
2. | Best Latch Possible
Of course any breastfeeding resource you read will talk about the “latch” and getting it right. So what is a good latch? A good latch is one that doesn’t hurt and one that helps the baby drink well! The following guidelines can help get you there:
Support the baby in a way so they can reach for the breast. Reaching will open the jaw wide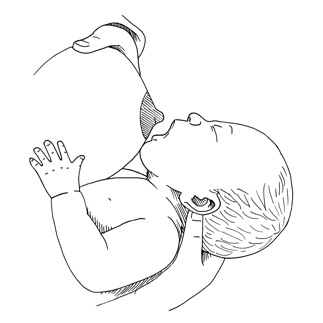 and allow for more breast tissue into the baby’s mouth. This is a good thing because we want the baby to be able to compress their tongue on the areola and for the nipple to be placed far back in the infant’s mouth where it will be more protected. The baby should have his or her little chin lifted up far from his or her own chest, with the chin actually pushing into moms breast while the nose does not touch the breast. With the best latch possible, we then watch for whether the baby is actually drinking or not by the movement in their lower jaw. Quick up and down movements of the baby’s jaw are generally seen when no or very little milk is being transferred from the mother to the infant. A deeper drop down of the lower jaw (with a slight pause before it rises up again) tells us the baby’s mouth filled with milk and swallowed it. Breast compressions can help babies get those drinks when they are just nibbling away, and if that doesn’t help after a bunch of tries we switch to the other breast
and allow for more breast tissue into the baby’s mouth. This is a good thing because we want the baby to be able to compress their tongue on the areola and for the nipple to be placed far back in the infant’s mouth where it will be more protected. The baby should have his or her little chin lifted up far from his or her own chest, with the chin actually pushing into moms breast while the nose does not touch the breast. With the best latch possible, we then watch for whether the baby is actually drinking or not by the movement in their lower jaw. Quick up and down movements of the baby’s jaw are generally seen when no or very little milk is being transferred from the mother to the infant. A deeper drop down of the lower jaw (with a slight pause before it rises up again) tells us the baby’s mouth filled with milk and swallowed it. Breast compressions can help babies get those drinks when they are just nibbling away, and if that doesn’t help after a bunch of tries we switch to the other breast
3. | Be Kind!
You have never breastfed this baby before, nor has this baby ever breastfed before! Breastfeeding is a learned process that can take some time before you feel it is comfortably established. Something I talk to all moms about is the importance of BEING KIND TO YOURSELF! Remember, you are doing one of the most important jobs on the planet, but it’s also the hardest job. The way you measure progress, productivity, and success as a mom (especially a new mom) is about to shift so give yourself the space and time to adapt to all the changes and find your way
If you and your little one are experiencing challenges with breastfeeding, I encourage you to access the help of an IBCLC (certified lactation consultant). Do this early as they can help you assess the situation, rule out any other barriers (like tongue tie for example), and help you create a plan that will aim to move things in the right direction!
 Laura’s passion for the environment, global health, and maternal and newborn care led her down her path to become a Naturopathic Doctor and International Board Certified Lactation Consultant (IBCLC). After completing a Bachelors degree in psychology, she went on study Natruopathic Medicine at the Canadian College of Naturopathic Medicine (CCNM) in Toronto. It was during that time she was introduced to Dr. Jack Newman’s International Breastfeeding Centre and the amazing work they do to help families achieve their breastfeeding goals. Realizing Lactation medicine was the missing piece she was looking for in her training and understanding the value of qualified lactation support, she decided to enrol and complete the necessary steps to become an IBCLC.
Laura’s passion for the environment, global health, and maternal and newborn care led her down her path to become a Naturopathic Doctor and International Board Certified Lactation Consultant (IBCLC). After completing a Bachelors degree in psychology, she went on study Natruopathic Medicine at the Canadian College of Naturopathic Medicine (CCNM) in Toronto. It was during that time she was introduced to Dr. Jack Newman’s International Breastfeeding Centre and the amazing work they do to help families achieve their breastfeeding goals. Realizing Lactation medicine was the missing piece she was looking for in her training and understanding the value of qualified lactation support, she decided to enrol and complete the necessary steps to become an IBCLC.
Laura sees herself as a community mobilizer and humanitarian. While at CCNM, she was very fortunate to complete a clinical externship in Haiti at a birth centre through Naturopaths Without Borders. It was there that her desire to serve moms and babies grew, and where she saw the power of breastfeeding in decreasing infant morbidity and mortality. The clinical focus in her private practise is with women in the postpartum period, supporting their transition into motherhood, guiding them with feeding support, and promoting infant mental health. She has worked in Thailand as a private consultant and with the Bangkok Child Protection project, a UNHCR funded initiative through Jesuit Refugee Services, where she provided case work support, needs assessments, and health education to unaccompanied minors.
Laura currently calls Toronto home where she lives with her husband and their two young children. She sees patients part-time and is developing online courses for new parents. Her current course, Prenatal Breastfeeding Companion, is an introductory breastfeeding course for parents-to-be which goes over all the essentials and includes a Facebook support group for members. 15% of the profits made on the course are currently going toward an amazing NGO called Nurture Project International who are working in Greece to support safe infant feeding with refugee families.
References:
- Pediatrics
- June 2016, VOLUME 137 / ISSUE 6
- Swaddling and the Risk of Sudden Infant Death Syndrome: A Meta-analysis.
- Anna S. Pease, Peter J. Fleming, Fern R. Hauck, Rachel Y. Moon, Rosemary S.C. Horne, Monique P. L’Hoir, Anne-Louise Ponsonby,Peter S. Blair.
















