The origin of the term “Dry Needling”
Dr. Janet Travell, personal physician to John F. Kennedy, made popular the idea of “trigger points” (motor points) and “trigger point therapy,” where needles are inserted into painful, “knotted” areas of muscle tissue for the purpose of relieving pain and dysfunction. Because trigger point injection is understood to mean a fluid injection (for example, the injection of a steroid solution), Dr. Travell coined the term “dry needling” to differentiate it from “wet needling” (i.e. trigger point therapy).
Some say Dr. Travell reasoned that dry needling is not acupuncture due to the difference in needle gauge (thickness). Though in reality, dry needling technique is almost identical to acupuncture technique (including needle thickness, point location and method of stimulation), the practice of “dry needling” today does have a specific sports medicine connotation. The approach to treatment does not include traditional tongue and pulse diagnosis and the reasoning given for point selection is biomedical in nature, relying primarily on neurophysiological explanations for treatment.
Ancient Technique Explained by Modern Science
Though the languaging is different, we can see that the ancient technique of acupuncture is again explained and supported by modern science. In ancient and current acupuncture practice, “a shi” points are the term that Western-trained clinicians today call motor points.
The Huang Di Nei Jing, a Chinese medical classic written over 2,000 years ago, described needling tender points for the resolution of pain. These points called, “a shi” points, or “oh yes,” points refer to points where the patient exclaims, “oh yes,” in response to the practitioner finding a painful area.1
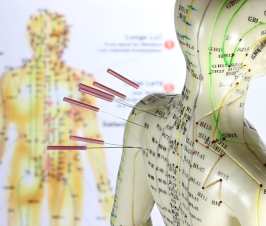
The most recent research shows a greater than 90% overlap between “motor points” and acupuncture points.2,3 Regardless of similarity, many clinicians today prefer to frame their practice either in accordance with Chinese medicine or with Western medicine terminology. My preference of course, is integration and unification of both. Anyone denying a significant overlap or the tremendous contributions of both Chinese and Western medicine would be doing a disservice to the field of pain management.
Motor Points in Practice
Inserting needles into motor points is now a common way of treating musculoskeletal injury and dysfunction. Though several methods exist for locating the “motor point,” most clinicians agree that eliciting a muscle twitch (LTR or local twitch response) in the affected area positively affects neuromuscular programming and restores the body’s natural baseline. The end result is resolution of pain and increased range of motion.
Even tendinitis and bursitis have been said to be well-treated through this method by re-balancing opposing muscle groups. One of the experts in this field, Matt Callison, LAc, has written several texts on motor points and sports medicine, integrating classical Chinese medicine with modern orthopedic approaches.
Amy Chong, acupuncturist and pain management expert in Seattle, WA, has found that trigger point therapy is frequently effective for “all types of myofascial pain, joint pain and restrictions, tendinitis, tendinosis, radiculopathy, headaches as well as for frozen shoulder, plantar fasciitis and TMJ (temporomandibular joint disease). The goals are more regional in focus rather than to aim for a systemic balancing effect, but the technique used is very similar to some of the classic techniques found in ancient Chinese medical texts.”
Regardless of how you say tomato, there is strong clinical support of acupuncture for pain management. Though getting acupuncture may initially require more time and money than taking a pain medication, the benefit of pain resolution without the common side effects of NSAIDs and corticosteroids is worth the investment. American medicine has an unfortunate tendency toward immediate results regardless of consequence. Many patients end up spending more time and money getting treated for the side effects of pain medications and have joints or organs that are worse for the wear.
References:
- Zhang SJ. [Origin and development of Ashi point location method]. Zhongguo Zhen Jiu.2013;33(2):165-7.
- Dorsher PT, Fleckenstein J. Trigger points and classical acupuncture points. Deutsche Zeitschrift fűr Akupunktur.2008; 51(4):6-11.
- Melzack R, Stillwell DM, Fox EJ. Trigger points and acupuncture points for pain: correlations and implications. Pain.1977; 3(1):3-23.