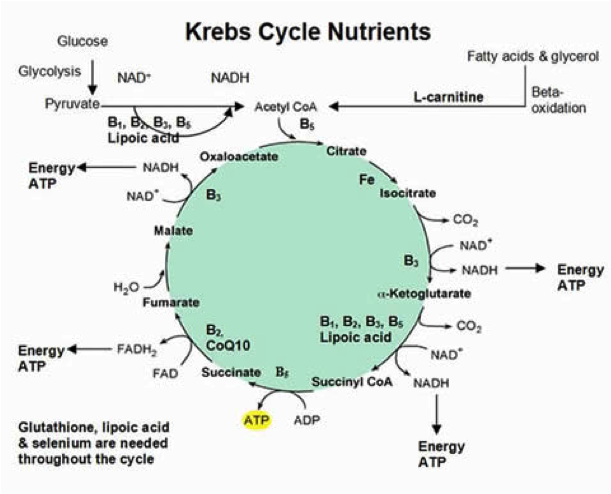
In the first part of The New Fibromyalgia, we looked at the history of Fibromyalgia Syndrome (FMS). We highlighted how the diagnostic criteria associated with FMS has changed over the years from requiring specific areas of tenderness or pain to diffuse pain as well the many comorbid symptoms and diagnoses, either in tandem with FMS or involved in its development. And finally we identified key nutrients involved in the Kreb Cycle that contribute to energy production in the cell.
Kreb Cycle
The Kreb Cycle is the energy cycle of the cell. Also known as the citric acid cycle, it the chemical process by which our food energy is converted to ATP- adenosine triphosphate, the chemical energy source from which all the body’s energy is generated. The Kreb Cycle takes place in the power plant of the cell, known as the mitochondria. Well-functioning mitochondria and a high number of mitochondria are both required for optimal energy production. Mitochondrial disease has been defined as a clinically heterogeneous group of disorders that arise as a result of genetic dysfunction of the mitochondrial respiratory chain.1 Therefore when ATP energy is not created properly by the cell it can be said there is mitochondrial disease1. In this article we discuss 1) a new theory for the evolution of the pathology may hinge on the health of the cellular mitochondria, 2) a theory that this controversial illness may be changing in it’s diagnostic criteria, as well as on the rise due the interplay between medical treatments, nutrient deficiencies and other comorbid lifestyle concerns.
The nutrients involved in the Kreb Cycle are essential for the production of ATP energy in the mitochondria. When this energy is not produced properly for any number of reasons, there is mitochondrial dysfunction, resulting in a lack of ATP production and accompanying symptomology of FMS; namely fatigue, muscle, nerve and join pain and stiffness. As FMS continues to better understood, what is becoming clear to some researchers and physicians is that the accumulation of causal factors and organ systems involved may have mitochondrial disease as a common denominator.2,3 At the cellular level mitochondrial disease can explain why the symptoms of fibromyalgia has be linked to numerous factors as vast as genetic predispositions, DNA malfunctions, Hep B vaccine4, HPV Vaccine5, cigarette smoking6, gluten sensitivity.7 In particular, however it is the use of some of the most commonly prescribed medications that could produce a similar symptom picture of FMS. At the cellular level, we all require oxygen, each of the micro (vitamins, minerals and amino acids) and macro nutrients (proteins, fatty acids and glucose) involved and indirectly involved in the energy or Kreb Cycle.
Chronic Fatigue Syndrome (CFS)
One study compared the mitochondria’s involvement in Chronic Fatigue Syndrome (CFS), FMS and normal healthy controls. Peripheral blood mononuclear cell showed decreased levels of Coenzyme Q10 from both CFS patients and FMS subjects and as well as decreased ATP levels for CFS patients and for FMS subjects, versus healthy participants. On the contrary, both CFS and FMS patients had significantly increased levels of oxidative stress-induced damage from lipid peroxidation. While the former findings overlapped between FMS and CFS, a key enzyme in the respiratory chain, mitochondrial citrate synthase activity was significantly lower in FMS patients whereas in CFS, it resulted in similar levels as controls. Additionally, mitochondrial DNA content was reduced in FMS patients as compared to normal in CFS and healthy controls. Epigenetic expression of mitochondrial illness pointed towards FMS but not CFS or healthy controls. These data lead to the hypothesis that mitochondrial dysfunction-dependent events could be a marker of differentiation between CFS and FMS, indicating the mitochondria as a new potential therapeutic target FMS in particular.2
CoEnzyme Q10
CoEnzyme Q10 (CoQ10) is the best studied Kreb Cycle nutrient for pain and myalgia. As we saw in the last study FMS patients have reduced CoQ10, a finding that has been duplicated by several studies. CoQ10 is a conditionally essential nutrient cofactor of the Kreb Cycle. It is made by the human body as well as sourced in small amounts from a variety of foods. As we age CoQ10 levels naturally depreciate. Some conditions of illness, stress and medications have also been shown to reduce CoQ10 levels. For instance, it has been a long-standing theory that statin-associated muscle pain (myalgia) is caused, or at least partly contributed by, a reduction in CoQ109,15 and L-Carnitine9 in muscle mitochondria. Myalgia or muscle pain is one of the main reasons why patients to either stop their statin or significantly reduce the dose of their statin.10,15 It is estimated that as many as 25% of statin users who exercise may experience muscle complaints due to statin therapy, which may be potentially dismissed by both patient and physician.15 Statin therapy has also been shown to cause muscle complaints in treated patients without inducing a marked increase in creatine kinase level.15 The clinical relationship between statins use with fibromyalgia are a concern for patients and physicians alike. In a large population health study, it was shown that 67% of Americans has high LDL (“Bad”) Cholesterol as of 2010, which is a continual upward trend from previous years.12 It was also assessed that approximately 24% of the American public is taking statins in order to lower LDL-cholesterol.12 Fortunately for millions of American, CoQ10 supplementation has been found to improve the patient experience of myalgia in statin-treated patients by reducing pain and restoring levels of deficient CoQ1010,11,13,14, in clinical trial.13Fortunately it has already been established that statin-treated women14 and adolescents15 with fibromyalgia as well as those labeled Statin Intolerant11 have been isolated as particularly benefiting from CoQ10 supplementation. The mechanism of CoQ10 for pain reduction may be via its regulation of inflammatory agents called inflammasomes whose increased presence in statin treated patients increases muscle pain and stiffness.17
CoQ10 is not the only nutrient associated with the FMS-type pain. The following nutrients, indirectly required for the Kreb Cycle.When trace minerals deficiencies were assessed for their coincidence with FMS, Low levels of magnesium and Zinc deficiency were associated with FMS with more tender spots being particularly associated with low zinc levels.18 Symptomatic myalgia in statin-treated patients with concurrent vitamin D deficiency may reflect a reversible interaction between vitamin D deficiency and statins on skeletal muscle.19 Non-specific muscle pains among Arab and Indian-Pakistani populations may indicate vitamin D deficiency, and prompt treatment can result in resolution of symptoms.20
There are still a lot of unknowns about FM, which is one reason why the diagnostic criteria has changed over the decades. As mitochondrial disease continues to better understood, what is becoming clear to some researchers and physicians is that the accumulation of etiological factors and organ systems can be condensed to the common denominator of the mitochondria. These power plants of energy, found in every body system and every cell type are a likely hinge on which FM manifests, which may account for the mysterious and elucive onset of FMS patients and its overall dismissal by many doctors in mainstream medicine.
 Dr. Millie Lytle is a Naturopathic Doctor and the founder of Nat Med Coach. She has a passion for finding and filling gaps of care in the health care system. She holds her license in the District of Columbia, practices virtually and in New York City. Originally from Canada, Dr. Millie earned her undergraduate degree from the University of Toronto, her doctorate from the Canadian College of Naturopathic Medicine and her Masters in Public Health from the Hamburg School of Applied Sciences in Germany. She is a published researcher, avid public speaker and author of Eating for Meaning. She is the director of Nat Med Coach and the founder of Virtual Health Club – providing supervised self-care to help you stay out of the doctor’s office. She sits on the Medical Advisory Board for the School of Applied Functional Medicine. Dr. Millie specializes in helping those address chronic fatigue with mind-body-spiritual well-being.
Dr. Millie Lytle is a Naturopathic Doctor and the founder of Nat Med Coach. She has a passion for finding and filling gaps of care in the health care system. She holds her license in the District of Columbia, practices virtually and in New York City. Originally from Canada, Dr. Millie earned her undergraduate degree from the University of Toronto, her doctorate from the Canadian College of Naturopathic Medicine and her Masters in Public Health from the Hamburg School of Applied Sciences in Germany. She is a published researcher, avid public speaker and author of Eating for Meaning. She is the director of Nat Med Coach and the founder of Virtual Health Club – providing supervised self-care to help you stay out of the doctor’s office. She sits on the Medical Advisory Board for the School of Applied Functional Medicine. Dr. Millie specializes in helping those address chronic fatigue with mind-body-spiritual well-being.
References:
- Chinnery P. Mitochondrial Disorders Overview. GeneReviews® [Internet]. June 8, 2000; Last Update:August 14, 2014
- Castro-Marrero J,Cordero MD, Sáez-Francas N, Jimenez-Gutierrez C, Aguilar-Montilla FJ, Aliste L, Alegre-Martin J. Could mitochondrial dysfunction be a differentiating marker between chronic fatigue syndrome and fibromyalgia? Antioxid Redox Signal. 2013 Nov 20;19(15):1855-60
- Cordero MD,de Miguel M, Carmona-López I, Bonal P, Campa F, Moreno-Fernández AM. Oxidative stress and mitochondrial dysfunction in fibromyalgia. Neuro Endocrinol Lett. 2010;31(2):169-73
- Agmon-Levin N,Zafrir Y, Kivity S, Balofsky A, Amital H, Shoenfeld Y. Chronic fatigue syndrome and fibromyalgia following immunization with the hepatitis B vaccine: another angle of the ‘autoimmune (auto-inflammatory) syndrome induced by adjuvants’ (ASIA). Immunol Res. 2014 Dec;60(2-3):376-83
- Martínez-Lavín M. Fibromyalgia-like illness in 2 girls after human papillomavirus vaccination. J Clin Rheumatol.2014 Oct;20(7):392-3
- Bokarewa MI, Erlandsson MC, Bjersing J, Dehlin M, Mannerkorpi K. Smoking is associated with reduced leptin and neuropeptide Y levels and higher pain experience in patients with fibromyalgia. Mediators Inflamm. 2014;2014:627041
- Rodrigo L, Blanco I, Bobes J, de Serres FJ. Effect of one year of a gluten-free diet on the clinical evolution of irritable bowel syndrome plus fibromyalgia in patients with associated lymphocytic enteritis: a case-control study. Arthritis Res Ther. 2014 Aug 27;16(5):421
- Valiyil R, Christopher-Stine L. Drug-related Myopathies of Which the Clinician Should Be Aware. Curr Rheumatol Rep. 2010 Jun; 12(3): 213–220
- DiNicolantonio JJ. Expert Rev Cardiovasc Ther. CoQ10 and L-carnitine for statin myalgia? 2012 Oct;10(10):1329-33
- Cordero MD, Alcocer-Gómez E, de Miguel M, Culic O, Carrión AM, et Can coenzyme q10 improve clinical and molecular parameters in fibromyalgia? Antioxid Redox Signal.2013 Nov 20;19(15):1855-60
- Kettawan A, Takahashi T, Kongkachuichai R, Charoenkiatkul S, Kishi T, Okamoto T. Protective effects of coenzyme q(10) on decreased oxidative stress resistance induced by simvastatin. J Clin Biochem Nutr. 2007 May;40(3):194-202
- Muntner P,Levitan EB, Brown TM, Sharma P, Zhao H, Bittner V, et al. Trends in the prevalence, awareness, treatment and control of high low density lipoprotein-cholesterol among United States adults from 1999-2000 through 2009-2010. Am J Cardiol. 2013 Sep 1;112(5):664-70
- Jacobson TA.Toward “pain-free” statin prescribing: clinical algorithm for diagnosis and management of myalgia. Mayo Clin Proc.2008 Jun;83(6):687-700
- Parker BA, Gregory SM, Lorson L, Polk D, White CM, Thompson PD. A randomized trial of coenzyme Q10 in patients with statin myopathy: rationale and study design. J Clin Lipidol. 2013 May-Jun;7(3):187-93. doi: 10.1016/j.jacl.2013.02.002. Epub 2013 Feb 26.
- Mascitelli L, Pezzetta F, Goldstein MR. Detrimental effect of statin therapy in women with fibromyalgia. Arch Intern Med. 2008 Jun 9;168(11):1228-9
- Miyamae T, Seki M, Naga T, Uchino S, Asazuma H, Yoshida T, et al. Increased oxidative stress and coenzyme Q10 deficiency in juvenile fibromyalgia: amelioration of hypercholesterolemia and fatigue by ubiquinol-10 supplementation. Redox Rep.2013;18(1):12-9
- Cordero MD, Alcocer-Gómez E, Culic O, Carrión AM, de Miguel M, Díaz-Parrado E et al. NLRP3 inflammasome is activated in fibromyalgia: the effect of coenzyme Q10. Antioxid Redox Signal. 2014 Mar 10;20(8):1169-80. doi: 10.1089/ars.2013.5198
- Sendur OF, Tastaban E, Turan Y, Ulman C. The relationship between serum trace element levels and clinical parameters in patients with fibromyalgia. Rheumatology International 2008 May 22
- Ahmed W, Khan N, Glueck CJ, Pandey S, Wang P, Goldenberg N, Uppal M, Khanal S. Low serum 25 (OH) vitamin D levels (<32 ng/mL) are associated with reversible myositis-myalgia in statin-treated patients. Transl Res.2009 Jan;153(1):11-6
- Clin Rheumatol.2009 Aug;28(8):971-3. Myalgias or non-specific muscle pain in Arab or Indo-Pakistani patients may indicate vitamin D deficiency. Clin Rheumatol. 2009 Aug;28(8):971-3
Photo by Kinga Cichewicz on Unsplash