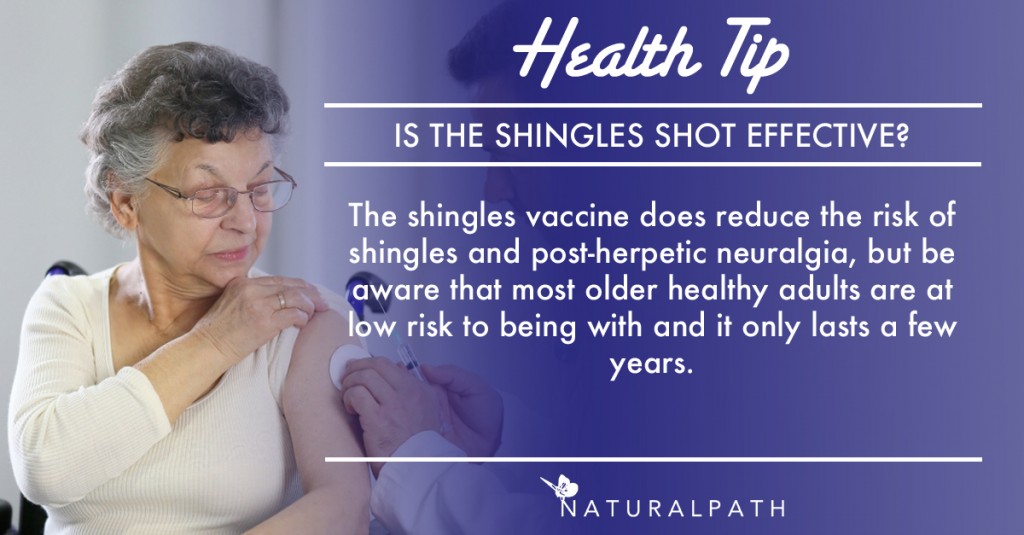
The last time you went to the pharmacy you were probably met with a large ad showing a person clearly in pain, exhorting you to get your shingles vaccine. No one wants to be in pain like that poor person in the picture, but it also makes sense to get the facts straight before asking for the vaccine, especially if you are under 60 and/or may have to pay for it out of pocket.
What is shingles?
Anyone who has ever had the chicken pox can potentially have shingles later in life. It is the same virus (herpes zoster), merely a reawakening that causes slightly different symptoms. Shingles causes a painful, blistering rash that typically takes two to four weeks to heal. It most commonly appears on one side of the torso and while not fun, usually heals without incident. It rarely appears in more dangerous places, like the eye, which requires urgent diagnosis and treatment. The biggest risk factors for getting shingles are age (it’s more common over the age of 60) and your overall health (being immunocompromised raises risk). In any given year your risk of getting shingles is less than ½ of 1% before age 60 and rises to as much as 1% by the age of 801. In less than 5% of all patients with shingles a secondary complication called post-herpetic neuralgia (PNH) arises that is potentially debilitating pain lingering after the rash has cleared.
What is the vaccine?
In 2006 Merck released Zostavax – the herpes zoster vaccination that protects against shingles. It is the only shingles vaccine currently available worldwide. It is most often recommended for patients over the age of 60, but is approved for ages 50 -59 as well. Long-term efficacy is still unknown and the goal is to use it for the population that is hardest hit by the disease, hence recommending it for patients over 60 who are more statistically likely to experience shingles. The CDC states that use of the vaccine reduces risk of getting shingles by 51% and of getting PHN by 67%. This statement is based on the Shingles Prevention Study2, a large study done following close to 40,000 patients for 3.1 years (median). A second study3 followed a subset of those patients (app 14,000) for an additional 4-7 years (and a further small subset even longer) which allowed the CDC to conclude that efficacy after 5 years in the population this is most indicated for (above 60) is not reliable. Note that data for patients above age 80 is minimal.
What are risks associated with the vaccine?
The shingles vaccine is contraindicated for anyone who has an allergy to any ingredient in the vaccine (including gelatin and neomycin, an antibiotic), anyone with reduced immunity such as cancer patients undergoing chemotherapy or radiation treatment, pregnant women, patients using steroid drugs, or patients with immune deficiency diseases such as HIV/AIDS. Zostavax is a live virus vaccine. Common side effects include soreness, redness, swelling or itching at vaccination site, headache. There is a new subunit (non-live virus) vaccine that is being studied that looks promising for greater immune response, even in immunocompromised patients, but is still in development and testing phase4.
Who should get the vaccine?
Immune compromise increases risk of herpes zoster. In patients with cancer risk is twice as high for patients with solid tumors and nearly six times as high for patients with hematological (blood) cancers5. Unfortunately, patients with hematological cancers or HIV are not eligible for live virus vaccines. Some people worry about whether they should get the vaccine after they’ve had an outbreak. For robust or normal immune systems the data is not compelling to vaccinate after one outbreak of zoster6 as the likelihood of recurrence is low, i.e. if you are an otherwise healthy person who gets zoster at age 60, that shouldn’t send you straight to the pharmacy for a shingles vaccine. In fact, there is an increase in humoral response after having shingles that confers immunity similar to if not better than the vaccine, so currently the recommendation is to wait a year after having had an outbreak of shingles before considering getting the vaccine7 so you get the most mileage out of your immune response.
 Another common question is whether we should simply administer booster shots at 5 to 10 year intervals, but it’s not yet clear if the immune system would actually benefit further by this or not. There is a clinical trial (sponsored by Merck) currently underway examining that question with a booster given 10 years after initial vaccination (ClinicalTrials.gov #NCT01245751). The trial is complete, but data have not yet been published.
Another common question is whether we should simply administer booster shots at 5 to 10 year intervals, but it’s not yet clear if the immune system would actually benefit further by this or not. There is a clinical trial (sponsored by Merck) currently underway examining that question with a booster given 10 years after initial vaccination (ClinicalTrials.gov #NCT01245751). The trial is complete, but data have not yet been published.
A critical factor when discussing vaccination in older patients is that the older a patient is the more vulnerable they are to disease and secondary effects (like PNH), but at the same time increasing age also decreases the efficacy of vaccination and at some point those two vectors cross and render routine immunization potentially ineffective. For now what we know about the shingles vaccine is that ii does decrease the incidence of shingles and post-herpetic neuralgia for at least 5 years in older adults, but for most people, your risk to begin with is pretty low. As a primary care naturopathic physician, I also stress when educating patients about shingles vaccination that non-pharmaceutical treatment is available and often quite effective at decreasing length of the outbreak and severity of symptoms which, sadly, does not come up in any of the research cited below. As always, talk to your physician to help make the best decision for your health.
 Dr. Alethea Fleming, ND is a passionate advocate for naturopathic geriatric medicine. A 2007 Bastyr University graduate, she also earned a certificate in Gerontology from the University of Washington. Dr. Fleming is the owner andleadphysician of the Vital Aging Clinic in Anacortes, Washington where she provides primary care to all adults as well as adjunctive geriatric care. Dr. Fleming is active in multiple community organizations as well as a member of WANP,AANPand OncANP. In her off hours, Dr. Fleming can be found hiking the beautiful trails of Fidalgo Island, spending time with her wonderful husband and son, or with her nose firmly in a good book.
Dr. Alethea Fleming, ND is a passionate advocate for naturopathic geriatric medicine. A 2007 Bastyr University graduate, she also earned a certificate in Gerontology from the University of Washington. Dr. Fleming is the owner andleadphysician of the Vital Aging Clinic in Anacortes, Washington where she provides primary care to all adults as well as adjunctive geriatric care. Dr. Fleming is active in multiple community organizations as well as a member of WANP,AANPand OncANP. In her off hours, Dr. Fleming can be found hiking the beautiful trails of Fidalgo Island, spending time with her wonderful husband and son, or with her nose firmly in a good book.
References:
- Kawai, K., Gebremeskel, B., Acosta, C.: Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014; 4(6): e004833.
- Oxman MN, Levin MJ, Johnson GR: A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med 2005;352:2271–84.
- Schmader KE, Oxman MN, Levin MJ, et al. Persistence of the efficacy of zoster vaccine in the shingles prevention study and the short-term persistence substudy. Clin Infect Dis 2012;55:1320–8.
- Lal H, Cunningham AL, Godeaux O: Efficacy of an adjuvanted herpes zoster subunit vaccine in older adults. N Engl J Med 2015;372: 2087–2096.
- Habel LA1, Ray GT, Silverberg MJ, et al.; The epidemiology of herpes zoster in patients with newly diagnosed cancer. Cancer Epidemiol Biomarkers Prev. 2013 Jan;22(1):82-90. doi: 10.1158/1055-9965.EPI-12-0815. Epub 2012 Nov 1.
- Tseng HF, Chi M, Smith N, et al.; Herpes zoster vaccine and the incidence of recurrent herpes zoster in an immunocompetent elderly population. J Infect Dis. 2012 Jul 15;206(2):190-6. doi: 10.1093/infdis/jis334. Epub 2012 Jun 4.
- Van Epps, P, Schmader, Kenneth E, Canaday, David H: Herpes Zoster Vaccination: Controversies and Common Clinical Questions.Gerontology DOI: 10.1159/000431374 July 16, 2015